THE ART OF HEALING
Soula Mantalvanos has been dealing with pelvic pain for over nine years. She's an aspiring creative living in Australia. An artist who battles Pudendal Neuralgia through her words & artwork. Soula's a die hard advocate for persistent pelvic pain sufferers. She's created an online communication tool called {Pain}Train to help those suffering from pelvic pain feel confident and empowered in managing their own pain journey. This unique communication tool allows you to share your information with just about anyone you want so there's no need to repeat yourself countless times.
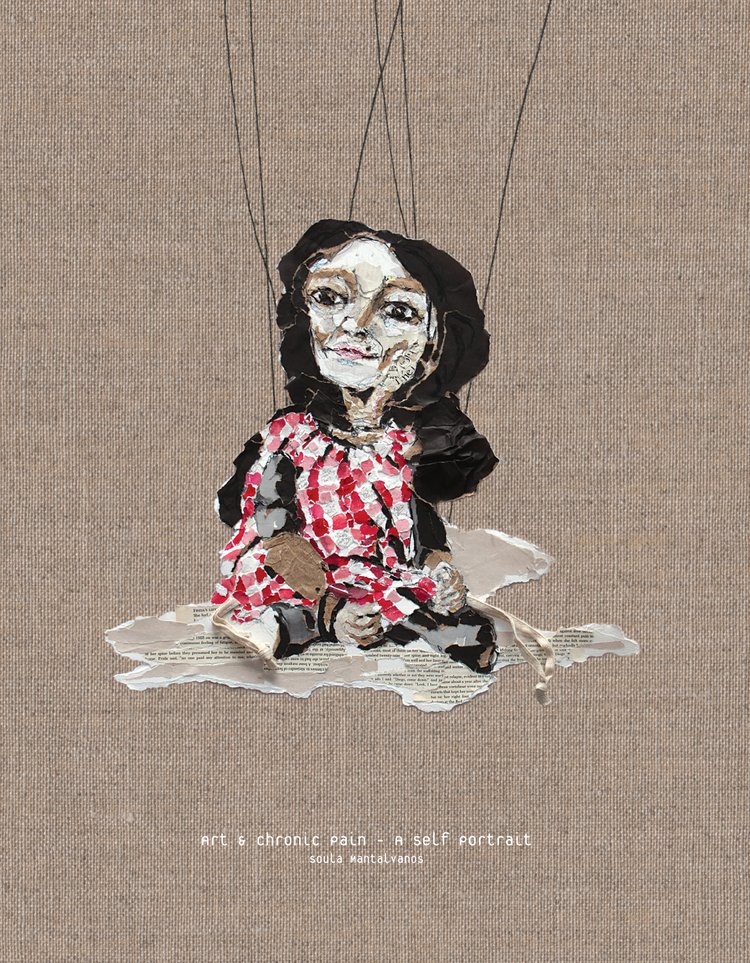
Soula's also the author of Art & Chronic Pain - A Self Portrait where she artistically expresses her experience with pelvic pain. Empathizing with others about the daily frustrations with "invisible pain." And she just doesn't stop there. You've got to check out her documentary, Hurting Strings and her Blog.
1. When did your journey with pelvic pain all start?
March 2007 when a fit ball (exercise ball) I was sitting on at my desk burst, and I dropped to a concrete floor.
2. Describe what your life was like before pelvic pain? After?
Absolute bliss, I had no pain. I worked full-time in my design company that I ran with my husband, Theo. I worked full days designing concepts for various clients. I had also just started to exhibit and had two exhibitions in the previous year and had two booked in for the following months. I practiced yoga four mornings a week; I walked everywhere, we lived in a central area so walked to shop, to dine, just for walking! We enjoyed annual overseas holidays and on the weekends, sometimes took off for long drives. We had a huge circle of friends, so our social life was very full. Life was full, fast, active and I felt I had no limits.
After eight weeks post-injury, I tried to stay positive assuming my injury was short-term. Instead, the pain was actually building and within eight months I had to stop working. Even during that time, I'd lie in the middle of our studio when the pain got too much, and then when I could handle the level of pain; I would resume working again. I just didn't think anything of it... until I had to! It was getting worse. The sensory pain and flares were becoming horrific. The toothache-like pain in my pelvis (more rectal area which is where I fell) was just excruciating, and I got to a point where the sensory pain became so unbearable I couldn't stand barefoot at all. I was on an electric vault and began to merely exist in a human shell. I shrunk to the smallest portion of myself; there was only a glimpse of me left. I didn't realize that was my lifeline and that spec by spec I would have to work my way back to being me again.
I know now, I'll never be me totally again, but I'm a lot more so. It was impossible for me to conceive that I could get back to where I am today. I felt life was over, and that life would end in that way, but I couldn't tell how long I would live. All I believed and was convinced about was that there was nothing but trying to get out of excruciating pain every second of the day. I lived second by second trying to manage.
I think of that now and honestly; I don't know how I made it through.
3. Can you describe your experience with the healthcare providers you met to help diagnosis you with Pudendal Neuralgia? How long did it take? How did you learn more about Pudendal Neuralgia?
I have THE most incredible Medical CV. I saw many reputable providers, there is no way I could comment on all of them, but I think I was caught in a kind of 'prehistoric Pudendal Neuralgia time.' I was also caught up in the Workers Compensation System which is the last thing you need with a chronic health condition - insurers love it when you have no evidence to prove yourself.
It took 4.5 years to be diagnosed, and that came after my first peripheral stimulation device was implanted - my neurosurgeon stating 'Where do you want me to start, there are so many nerves down there' when I asked about a nerve block. I also asked him to chop my coccyx off, and I'm very grateful that he advised for something less invasive first. That first implant saved my life. I could not stand or sit when I met him. He said what everyone had said to me- that I was the worst case he'd seen.
My diagnosing physio took all of about 10 minutes to make the diagnosis, and I will never forget the feeling that someone finally spoke my language. We were communicating, she understood everything I described and even had a name for it. 'Sensory pain,' 'delayed pain response,' 'hypersensitivity,' were all terms I had never heard until that day. And I finally had the courage to talk about this fabulous denim skirt that I wore that for some reason reduced my pain levels. I could never have brought that up with a previous provider, they looked at me strangely when I described the chronic pain, but Anne-Florence Plante asked that I wear it next appointment. She took one look at it and said, 'one moment' and ducked out of her office returning with a pregnancy belt. She knew straight away the skirt had support where I needed it. Finally, confirmation that I wasn't mad. Confirmation that weight = pressure on the nerve, that being in water DID cause pain, that sounds can cause pain, that being in a busy place can cause pain and fatigue, that sitting could be unbearable, that my toileting function and signals were out of whack, and so were the sexual functions and signals, that chronic pain was exhausting and fatigue was part of it... I could go on.
I learned much more from Anne-Florence who tapped into my professional design skills (all of which I could apply in 5min intervals and total just 30 mins a day) and requested that I build a website to help others. She came to my home and dropped all her research and notes taken from every lecture she'd been to and said 'here, you can do it.' I contacted everyone in her notes to ask permission to use their research on the website. They not only gave me permission but encouraged me to do so adding links to their sites and this stay still following the blog and occasionally sending me personal messages of thanks.
4. How did pelvic pain change your sexual function and intimacy with Theo?
Pelvic pain is like a switchboard that slowly switches off your life. From my basic sitting ability to managing my home and working ability and then to my personal and sexual functionality and need/want for intimacy and even need/want for a basic get-together or outing, it's all affected in the same way. It is all difficult to approach, manage, and to participate. I need to push passed the pain barrier first, then how many times can you say 'ouch' or 'not there' or 'not like that' etc. it kills the moment and of course, facing the pain afterward is another issue. Together, Theo and I have learned the limitations, we know what not to do, but the pelvic pain has stolen our spontaneity and freedom. I can thankfully report that I no longer have the torturous clitoral stimulation, but I have a lot of spasming.
5. How did Theo react to your initial experiences of pelvic pain? How did he feel?
Theo has supported me 100% from day 1. He is devastated but we work at it together. It's the only way to manage if you choose to stay together. It takes two people to get me through the day.
Theo: I was unaware of pelvic pain and put the pain down to what we call lower back pain.
6. What treatment(s) have you tried for pelvic pain? What helped? What didn’t?
There isn't much I haven't tried, and mostly I've tried various therapies with various treaters. My remedial massage helped immensely, and I kept that up for eight years. The biggest treatments were a diagnosis, removal of a pelvic ligament (which I believe could have been avoided if I'd been appropriately diagnosed), nerve blocks to the pudendal nerve (rectal branch), and above all, the two stimulation implants.
Water therapies were out of the question. The water is just too much pressure on the pelvis. Floating is lovely, but then I need to get out of the water! Also squeezing, tightening, and strengthening activities. I need 'opening,' 'releasing,' 'breathing' activities. Anything that translates to pressure or weight doesn't seem to work.
Also, the insurer appointments with treaters that can't rate pain as a disability were aggravating and infuriating. And of course, all the 'professionals' out there who don't keep up with their education and won't refer you to someone who does.
7. Please describe your experience with pelvic floor physical therapy. What did you find most helpful?
I haven't done much pelvic floor physical therapy. I flare straight away with the internal contact. I found Amy Stein's DVD and belly massage helpful.
8. What were some of the struggles you had with pelvic floor physical therapy?
The flare, it's just impossible. I persisted too but didn't find a way.
9. What was the worst advice you received about your pelvic pain? The best advice?
Worst advice was no advice for 4.5 years. The best advice was the diagnosis. It gave me a path, a lead. I was lost before that and heading down hill very fast. I keep recalling two quotes from professionals (one an alternative medicine practitioner and one a pain specialist): Your initial injury is a shock to the nervous system' and 'you're feeling things you shouldn't feel.' It makes me feel 'ok' and that there is no danger. It calms me and removes the 'it's all in your head' talk I heard.
10. When did you start to begin to feel like yourself again?
Probably in the last two years, I have begun to recognize myself again. The stimulation devices and appropriate treaters have helped. Sadly though I am letting go of who I was and realizing I have to make a new me.
11. How did pelvic pain shape who you are today?
I've learned that we have to remain grateful and understand that life is made of all things. We have to be responsible for our life and what happens and remember that we are not entitled to a better life than anyone. I've learned a lot about ego and believed that if we learn to manage it (put it away mostly!) that we make better people. I don't mean put away confidence or pride, but ego - it's different. What I'm getting at is the 'Why me?' question. Remove that, and it's part of the treatment I think!
12. How is your relationship with Theo now? Is there anything that you're still working towards?
It's great; it's always been great. It is still growing which is incredible given the difficulty. I'm always hopeful we can be more intimate and more spontaneous. We are very close and have a wonderful relationship but a chronic health issue does impact it, and at times I just feel very sad.
13. What advice would you give to the loved ones of those who have pelvic pain?
I couldn't give advice. It's different for everyone. I understand if people can't stay together, I get it; it's too hard. If you can grow through a health issue, it's a great credit to you, but sometimes I do find myself thinking, Theo could have a better life. Other times I feel, there will always be something to manage in life and that we should stick it out and keep fighting the monster that intrudes all the time.
Theo: You may not understand it, but you should believe the other person when they express that they are in pain. It is very difficult to sympathize when you can’t relate. I have never broken a bone in my body so I cannot comprehend what type of pain is experienced from a broken bone. Another example, a woman cannot sympathize with what it is like to be hit in the testicles, but experience shows that they believe it to be of an extreme level.
14. What inspired you to create a blog about pelvic pain and write a book?
I wanted to help others and save them the 4.5 years it took me to find a diagnosis. I've learned so much and to keep that to myself makes no sense. I also find a lot of release in expression. As an artist I love characterization, and the more eccentric the character is, the better, so it was a creative challenge for me to document and communicate the 'Soula in pain' character. The book is snippets from my posts so not really 'a novel' or anything, but I wanted it that simple to communicate the pain and experience in a simple manner that others could understand. A chronic pain patient's coffee table book if you like. Also, a way for me to be with others... everyone can have a little piece of Soula. Theo attached all the strings one by one!
15. Who or what has been your greatest inspiration and gift of hope?
I think about that often, what keeps me going and I draw a lot from artists, Frida Kahlo in particular, but at the end of the day, I believe we are the ones who keep ourselves going. There are the little things that make a difference to you (like someone sending you a nice email, or leaving a note in your letterbox - could be anything) but the fact that it means so much to you, means you're open to it, and you're looking for it. So 'you' do it. 'you' keep 'you' going.
When I was in the thick of it and was living minute to minute trying to get out of that horrendous pain, I remember thinking there's one glimpse of Soula left. I'd pick up my phone (it was too heavy for me most times), but I'd take one image and Instagram it. It was a little creativity... a little piece of Soula. From there, step by step I made it back slowly. I've also begun to make a new Soula.
16. What are some resources that you've found to be most helpful?
John Quintner has taught me so much about pain.
I'm subscribed to Body in Mind
Lorimer Moseley is incredible and led me to my diagnosing physio after reading one email!
I've read and followed Norman Doidge's books and findings.
My pain specialist has incredible resources and is a huge strength vicpain.com.au
I think above all, Theo and creativity have helped me the most.
17. What advice would you give to someone who's just started experiencing pelvic pain?
To take charge, take it on like it's a heart condition and be in control - don't wait for someone else to manage the issue. That's how you'll find the right people and become the best you can be.
Hopefully, resolve it if it's early days. If they need a pain profiling tool then they can use my pain-train.com.au
This information is not intended to substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of a healthcare professional with any questions you may have regarding treatment, medications/supplements, or any medical diagnoses. This information is intended for educational purposes only and is in no way to substitute the advice of a licensed healthcare professional.